Diverticular Disease: What has changed
in the last 25 years?
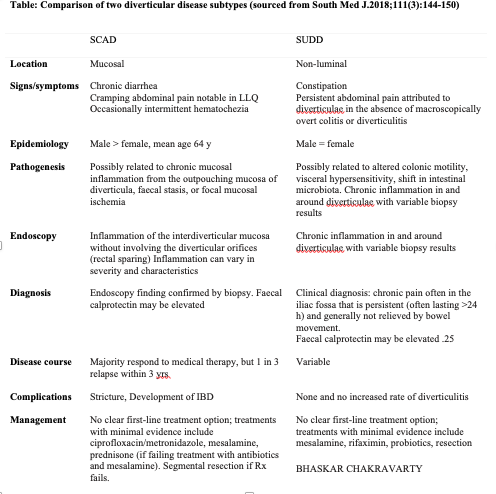
We have learned of atypical forms of diverticulitis such as segmental colitis associated with diverticulitis (SCAD) and symptomatic uncomplicated diverticular disease (SUDD). Additionally, we’ve learned of the role of prophylactic therapies such as fibre, probiotic, prebiotic etc. and we also address the role of antibiotics and post diverticulitis colonoscopy.
Prevalence: 41.7% and increases by 25% with aging.
Diet: fibre derived from vegetables, fruits and a diet low in red meat and fat is associated with less diverticular complications.
Caffeine, alcohol and smoking can be associated with more complications. Running and Jogging is associated with decreased risk of diverticular complications.
Obesity is associated with increased risk of complication particularly in women with BMI greater than 30. Low Vitamin D can be associated with worse outcome such as abscess.
SCAD presents with diarrhea, bleeding and cramps. There is interdiverticular mucosal inflammation. Variably responds to ciproxin, metronidazole, mesalamin and prednisone. Can develop stricture or inflammatory bowel disease long term.
SUDD is characterized by pain, constipation and chronic inflammation in and around diverticuli. Elevated faecal calprotectin is seen on occasion. Treatment is with mesalamine, rifaxamin, probiotics and surgical resection.
Prophylaxis and treatment summary:
- Increased fibre consumption reduces risk of diverticulitis.
- Mesalamine reduces risk of recurrent diverticulitis in SUDD patients.
- There is data to suggest reduction of diverticulitis recurrence with combination treatment of Rifaxamine and increased fibre consumption.
There is evidence now that majority of uncomplicated diverticulitis can be treated without antibiotics. The American Gastroenterological Association supports this position; however, the American Society of Colorectal Surgeons still recommends antibiotic treatment in this situation but recommends surgery be used in complex cases such as those with abscess.
Colonoscopy is still recommended in 4-8 weeks post-diverticulitis to rule out bowel cancer (1.1%) or advanced adenoma (3.8%)
Reference and recommended reading:
South Med J.2018;111(3):144-150